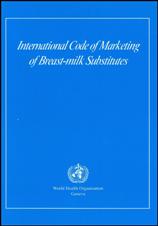
 The World Health Organization (WHO) International Code of Marketing of Breastmilk Substitutes is intended to protect and promote breastfeeding by preventing the inappropriate marketing of breastmilk substitutes, bottles and nipples.
The World Health Organization (WHO) International Code of Marketing of Breastmilk Substitutes is intended to protect and promote breastfeeding by preventing the inappropriate marketing of breastmilk substitutes, bottles and nipples.
There seems to be a lot of confusion however about what this actually means, and why it is important. The WHO code does not prohibit the sale or use of formula, bottles or nipples. It is not a statement that moms who use formula or bottles are bad moms, and it is certainly not a statement that formula is evil. The WHO code simply deals with the way the products covered under the code are marketed. This is important, because whether we want to admit it or not, we are all influenced by the marketing that happens all around us every day. There are those who feel that they are smart enough not to fall prey to marketing, but formula companies spend millions of dollars on marketing every year, and they would not be doing so if it didn’t work. I have blogged before about the subtleties of formula marketing, and ALL of us are vulnerable. Marketing of formula, bottles and nipples, has a negative impact on breastfeeding initiation and duration, and there are 30 years of research to back that up. The WHO code is an important document that is sound in theory, but seems to have little impact in practice. Why is that?
The answer is simple. Following the WHO Code is voluntary, and following it means limiting marketing and potential sales, so why would any company want to? The way things stand right now, it is not in a company’s best interest to be compliant with the WHO code. Since compliance is voluntary, and most companies have no interest in complying, those companies who do try to comply are put at a disadvantage.
Evenflo decided to try being WHO code compliant, and subsequently became the first bottle manufacturer to gain compliance with the code. This was a wonderful accomplishment, and it shows that it is possible. Recently however, they backtracked on that commitment and they are no longer compliant with the WHO code. Although I do not like the recent changes at Evenflo, I do understand why they happened. Evenflo (and other companies like them) are for profit companies. They exist to make money, and they answer to their shareholders. Following a code that limits the marketing of their products results in lost sales, and if their competition is not following that same code, it’s inevitable that eventually market share is going to become more important than upholding the WHO code.
The WHO code is great in theory but with no legislation behind it to force compliance, it is never going to be effective. Until the government gets serious about supporting breastfeeding and makes it a requirement for all companies, doctor’s offices, etc to be compliant with the code, there will never be any real change. I feel that when we see companies who are not complying with the code we should provide feedback to the company, but at the same time we need to be directing more of our energy towards putting pressure on our government. There will not be lasting change until governments decide to get behind the WHO code and make it mandatory to comply with it.